Search Posts
Recent Posts
- Equine Stress Relieved by Specifically Designed Music March 29, 2024
- Summer 2016 July 3, 2019
- Quantitative Fecal Analysis July 3, 2019
- 10 Tips for Caring for the Older Horse July 3, 2019
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.

Summer 2016
PUBLISHED BY EAST COAST EQUINE VETERINARY SERVICE
PO BOX 91 33B KENNEDY RD, TRANQUILITY, NJ 07879
PAUL ZIMPRICH, DVM ALEX CIUFFITELLI, VMD ANDREA BUTTERFIELD, DVM
A Tale of Two Alexs
Have you called the office recently and heard “Alex” answer the phone thinking it is Dr. Alex? We now have TWO Alexs. Dr. Alex Ciuffitelli and Alex Fezenko. Many of our clients have met Dr. Alex and have had her treat their horses. Alex Fezenko originally worked for her father’s practice, Tranquility Large Animal. She took the past four years off to raise her children and rejoined the East Coast Equine Team in March of 2016. We are excited to have Alex back in the office! Be sure to give Alex a warm welcome back next time you call the office.
East Coast Equine Dental Services
What to Expect from your Dental Exam Equine dental care can be provided in the field. Our staff is equipped with the latest in digital radiography and equipment. This equipment, when coupled with our training and experience, allows us to provide unparalleled equine dental care.
Your horse’s dental care is essential to your horse’s wellbeing. Regular examinations and maintenance on their teeth is especially necessary for today’s horses. Maintaining your horse’s proper dental care has its rewards with a longer more comfortable future. With proper dental care your horse can utilize feed more efficiently, maintain proper body weight and carry a bit more comfortably when bridled.
Floating Your Horse’s Teeth: The floating procedure is only one aspect of a complete dental examination. A full evaluation of your horse’s teeth should be done yearly, but in some cases a more frequent exam is necessary. Sharp points occur in most horses over time due to uneven grinding and wear on the horse’s molars.
Floating your horse’s teeth is rasping or filing the teeth. Floating removes sharp enamel points. These enamel points cause considerable discomfort to the cheeks, gums and tongue. The most common tools used are floats. Floats are long handled rasps that are designed just for filing down the teeth. Recently with the advent of motorized dental equipment, ECEVS veterinarians are equipped to meet all of your dental needs. There have been many exciting advances in equine dentistry over the past five years that have revolutionized our ability to provide the highest level of dental care.
What to expect during your horse’s dental float:The overall process usually takes about 45 minutes. This time includes examination, sedation, record completion, and client discussion. Horses with serious abnormalities, those who are extremely resistant, or those requiring additional diagnostics will take longer. ECEVS veterinarians are very careful to let the horse periodically rest during long procedures. It is not safe to keep the mouth open wide for long periods of time without a break.
Exam– A complete physical examination will be per-formed. The eyes and skin will be examined for any abnormalities. A stethoscope is used to listen for heart murmurs or abnormalities in the intestinal tract.
Initial Dental Exam (pre-sedation) An initial dental exam is performed. The head is palpated for any painful areas or asymmetry. The temporomandibular joints are checked for abnormalities or pain. The forehead and cheek muscles are examined for symmetry. Sensitivity from cheek pressure can indicate sharp points. Incisor alignment and freedom of movement is assessed. The jaw is moved from side to side to assess mobility. A distinct sliding sound can be heard, and the character of the sound can indicate dental abnormalities. The front cheek teeth can be assessed for abnormalities.
Sedation– Your horse will be sedated to make your horse feel relaxed. The medications used act quickly and wear off in 30 to 45 minutes. Sedation is necessary to perform a thorough examination and comprehensive dentistry.
Speculum– A speculum will be placed in your horse’s mouth. This keeps the horse’s mouth open during the exam and floating procedure The combination of a speculum and magnetic oral light allows for a thorough visual exam of the equine mouth.
Dental Exam (post-sedation) – A thorough examination of all 24 cheek teeth can now be completed. The cheek teeth are assessed for steps, waves, exaggerated transverse ridges (exaggerated roughening of the chewing surfaces), dental decay, fractured teeth, and various other abnormalities. The bars of the mouth (the space between the cheek teeth and the incisors) are evaluated for biting injuries and wolf teeth.
Hand float & Power float– ECEVS veterinarians use a combination of motorized and hand tools to best address your horse’s needs. Motorized equipment includes both rotary and reciprocating instrumentation. This broad selection of instruments allows pin point accuracy. ECEVS veterinarians can address each portion of each tooth individually as they work to make the whole mouth a smoothly functioning unit. A scaler is used to remove Tarter at this time if needed.
Post-Float– Under most circumstances, horses may be ridden as normal the following day. Your horse should not eat hay or grain for at least 2-3 hours after a sedation and dental procedure. Once they are fully awake, most horses never miss a meal. A few horses seem to be sensitive to even minute changes in their mouths, even if the changes are for the better. These patients may require a day or two to adjust to their new bite. Your ECEVS veterinarians are available and happy to address any concerns at any time following the procedure.
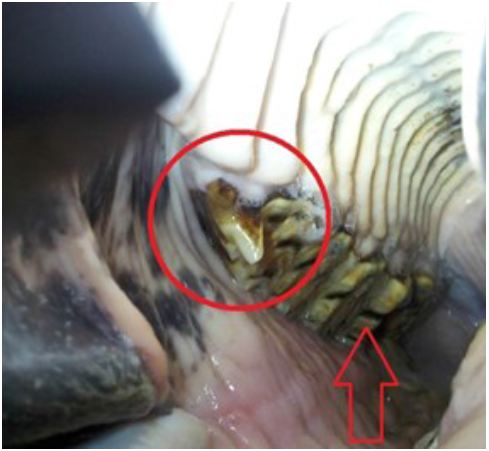
Before Dental Float: Notice the sharp hook on the 2nd premolar circled in the above photo and the unevenness of the teeth indicated by the red arrow

Post Float: Sharp hooks have been removed and stepping has been corrected.
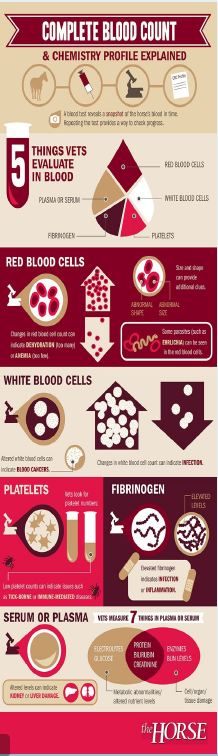
In –House Lab
ECEVS has the ability to run CBC/Chem in-house. This allows ECEVS rapid turnaround for blood results, diagnosis and possible treatment. Blood testing is commonly used to help diagnose illness or injury in horses. It can also help determine the state of your horse’s health during regular physical exam visits. Although a CBC or a chemistry profile can be performed separately, these tests are frequently done at the same time; when the results are interpreted together, they provide a good overview of many of the body’s functions. Your veterinarian will combine test result information with physical exam findings, medical history, and other information to assess your horse’s health status and determine if additional testing should be recommended. CBC/Chem test results tell a veterinarian what is going on in the horse’s bloodstream at the time the blood was drawn. What is in a CBC/Chem you might ask or what is my veterinarian looking for? Red Blood cells, white blood cells, serum, and platelets counts are the 5 blood components that a veterinarian will look at. The numbers, shapes, and sizes of blood components can tell a veterinarian if a horse is possibly anemic, losing blood, is dehydrated or fighting an infection. The Chemistry profile is a panel of tests that analyzes organ function (kidney, liver, etc).
Is a pre-purchase Exam worth it?
By: Dr. Alex Ciuffitelli
When purchasing a new horse, the first question is “Will this horse and I make a great team?”, and after you realize that you found a match made in heaven, the next big question arises – “Are there any health issues I should be concerned about?” This is where a pre-purchase exam, or a “vet-check”, comes into play. A pre-purchase exam is an evaluation of the horse performed by your veterinarian that helps determine their current health status and find any possible problems, whether they are affecting the horse now or may be a problem in the future. When per-forming a pre-purchase, each body system is carefully evaluated for abnormalities. Your veterinarian will look for problems such as cataracts when evaluating the eyes, arrhythmias or murmurs when listening to the heart, evidence of heaves when listening to the lungs, and signs of old injuries and current lameness when evaluating the limbs and feet, in addition to many more! Obviously, your veterinarian cannot foresee every problem that will occur, but they can help you identify current concerns and give you a better prognosis for the future soundness and health of your prospective new horse.A typical pre-purchase exam will begin with a complete physical examination of the horse, looking closely at their eyes, listening to their heart and lungs, and palpating everything from their poll to their hooves. Their overall conformation is assessed and they are observed for abnormalities in their demeanor or stance. A lameness evaluation is then performed in which each limb and joint is evaluated for signs of previous injury, such as a thickened tendon or joint effusion, and cur-rent lameness through observing the horse in motion and flexion of each joint. Although there may be underlying abnormalities not made evident through this thorough ex-am, many problems can be caught early and your veterinarian can ex-plain the long-term effects and what to expect in the future. After a thorough physical examination, your veterinarian will make recommendations based on their findings to per-form additional diagnostic such as radiographs, ultrasound, endoscopy, bloodwork, and drug testing. Often times, owners and veterinarians will agree to perform surveillance radio-graphs of areas that are predisposed to having diseases that may not show up on physical exam, such as the feet and hocks. This is done particularly when there is a breed disposition or conformational ab-normality, such as navicular disease in quarter horses, or the horse will be expected to perform at a high level and problems such as osteochondrosis dissicans (OCD) should be ruled out. Many owners will request a drug screen to detect anti-inflammatories or tranquilizers that may be in the horse’s system. Basic bloodwork including a complete blood count (CBC), chemistry panel, and fibrinogen is often per-formed as well to not only detect current issues, but to have as a base-line in the case of future illness.
Pre-Purchase exams are an important part of purchasing a new horse to not only help find health issues but to also help save money and stress down the line in finding problems that may not be evident to the untrained eye. Pre-purchases can be specifically catered to each individual horse and budget. It is important to remember that a pre purchase exam cannot always find every small problem and it cannot predict all problems that will arise in the future, but it provides you with a host of information on your prospective new horse and aids in the decision making process of the purchase. If you have any questions regarding pre-purchase examinations, please don’t hesitate to contact one of the vets at East Coast Equine!
The hock radiograph (pictured to the right) reveals a large osteophyte at the tarso metatarsal and there is fusing of the distal metatarsal joint.

Equine Emergencies 101
Equine medical emergencies happen. Even the most experienced horse owner faces equine medical emergencies whether it is a simple episode of colic or a laceration. As a horse owner, you must know how to recognize serious problems and respond promptly, taking appropriate actions while awaiting the arrival of your veterinarian.First and foremost, it is important to know how to T. P. R your horse and know YOUR horse’s “normal”. What is TPR you ask? T is for temperature. A normal temperature ranges from 99.5-101.5 degrees Fahrenheit. A horse’s temperature is taken rectally. P is for pulse rate. A horse’s normal pulse rate is 30 to 42 beats per minute. R is for respiratory rate. A normal respiratory rate is 12 to 20 breaths per minute. It is recommended to know these values for your horse in a normal relaxed state. Write them down and keep them in your barn first aid kit.
First Aid Kits
Here is a list of some essential items for your barn first aid kit.
- Cotton roll
- Cling wrap
- Gauze pads (assorted sizes)
- Gauze wrap
- Vet wrap
- Elastikon
- Bandage scissors
- Thermometer
- Betadine Scrub
- Antiseptic
- Latex gloves
- Flashlight and extra batteries
- Emergency contacts

Common Equine Emergencies Colic:
Colic is a broad term referring to gastrointestinal discomfort. Types of colic are: gas bubbles or “gas colic”, impaction colic, Twist, displacement or Bowel rupture. Common causes of colic include: inadequate water intake, changes in diet, extreme or adverse weather changes, grain overload, consumption of sand or bedding materials, stress, parasitism, or poor dental condition.
Clinical Signs: pawing, sweating, not eating, looking at sides or belly, biting at their sides, flank watching, lip curling, stretching out, restlessness (laying down and getting up), and rolling.
What to do: Call your veterinarian. Remove all food from the stall, if horse is standing or laying quietly this is OK as long as the animal is not rolling or thrashing. Be sure to monitor the horse. If the horse will not stand or lie down quietly hand walk for 20 minutes or until the veterinarian arrives.
Choke:
Also known as Esophageal Obstruction. Occurs when feedstuffs become lodged in the esophagus and the horse cannot swallow. Causes of choke are eating too fast, poor dentition, failure to soak feed adequately, feeding rough poor quality hay, or esophageal abnormalities.
Clinical Signs: Feed material (usually green in color) and/or saliva coming out of one or both nostrils, retching, coughing, and agitation. The horse may have a visible/palpable protrusion on left side of neck.
What to do: Don’t Panic! Call the veterinarian immediately. Remove water and feed from your horse’s stall. Keep the horse quiet no walking or lunging until your veterinarian arrives. Your veterinarian may sedate your horse and pass a stomach tube to resolve the obstruction. Aspiration pneumonia is a common complication of choke. This is a very serious condition. It is advised to monitor your horse’s temperature daily for one week after a choke episode.

Opthalmic Emergencies:
Eye injuries should ALWAYS be considered an emergency! Common eye problems include: uveitis, blunt trauma, corneal abrasions or ulcers.
Clinical Signs: Call your veterinarian immediately if you observe any of the following: a swollen eyelid, excessive tearing or drainage, squinting, cloudiness, redness, laceration or penetrating wound of the eye.
What to do: Call your veterinarian. It is important NOT to self-treat eye problems. For example a topi-cal eye ointment with a steroid is not appropriate if there is a corneal ulcer. It is best to allow your veterinarian to exam the eye and make the appropriate diagnosis.

Lacerations:
These injuries should be treated immediately! If you find your horse with a laceration, ask yourself the following questions: is my horse in immediate dis-tress? Is there active bleeding? Is the wound near a joint or tendon sheath? The sight of a laceration can send any horse owner into dis-tress, but please DON’T panic! Try to stay as calm as possible to assess the situation.

What to do: If there is active bleeding, stop the bleeding by applying direct pressure or a pressure bandage. DO NOT remove the bandage once applied. If it becomes saturated, simply add more layers. Run cold water over the laceration. DO NOT apply a tourniquet or any ointments!
When you call the veterinarian, please have the following information available: The location of the laceration, the depth of the laceration (is bone visible?), is any lameness associated with the laceration, and is the horse in a safe contained location.
Suture care is an important part of the healing process. Please be sure to follow your veterinarian’s treatment plan to ensure proper healing. Make sure sutures are kept clean and watch your horse! Healing wounds start to itch! If you notice your horse rubbing or scratching his or her sutures take immediate action. It is not uncommon for a horse to rub out their sutures and this may require the veterinarian to re-close the wound and delayed healing.

Sudden Onset Of Acute Lameness:
Sudden onset of acute lameness is a broad category. These injuries are encountered fairly often and include nail punctures, hoof abscess, laminitis (founder), and even fractures. Joint and tendon injuries can occur in both performance horses, in stall/barn accidents, and in horses housed in open pastures. If your horse was fine yesterday, and dead lame today, do not delay in seeking professional help in diagnosing and treating the condition.
What to do: Examine your horse for any wounds, heat or swelling in the affected limb. Check the foot for any penetrating wound (i.e. a nail in the foot) or problems with a shoe. Should you find a nail or foreign body in the hoof DO NOT try to remove it! The veterinarian will want to see the location of the foreign body and possible take radiographs to determine exactly what structures of the foot are involved. If your horse is willing to walk, get him or her to a safe place. If the horse is resistant to move, do not force them to move! Check your horse’s temperature. The presence of a fever with acute onset of lameness is of significant concern. This information will allow the veterinarian to determine the best course of action. Cold hose the injury until the veterinarian arrives. DO NOT administer bute or ban-amine. These medications mask pain and fever potentially hindering an accurate diagnosis. Upon arrival, the veterinarian will perform an exam and possible take radiographs or ultrasound images.

Fever:
The normal temperature for a horse is 98.5-101.5F. If your horse seems depressed, lethargic, not acting him/herself and is not eating, the first step is to take his temperature. This information is extremely helpful for our office staff to relay to the veterinarian when there is an emergency. Fever can be an indicator of infectious diseases or tick-borne disease. Your veterinarian will ask if the horse has left the farm recently or been exposed to other horses that have been sick.

Allergic Reactions:
Horses can have allergic reactions to many things including but not limited to dust, mold, feed ingredients, insect sprays, insect stings/bites, and medications or supplements. Just like in humans, reactions can be mild hives to anaphylactic shock.
Clinical Signs: Hives in patches of the body or all over the body (mild reaction), swelling of the eyelids, muzzle or head, difficulty breathing and/or fever are signs of a severe reaction and possible anaphylaxis and should be seen immediately!
What to do: Cold hose the horse to cool the itching of hives and reduce fever of a severe reaction. In the case of a severe reaction keep the horse calm until the veterinarian arrives. Mild reactions such as hives can be treated with IV steroids as well as oral powdered steroids. Anaphylaxis requires more aggressive treatment with epinephrine, DMSO, and IV fluids and may require the horse to be hauled to an emergency clinic.
Laminitis:
Laminitis also called “founder” inflammation of the laminae in the hoof. The signs of laminitis may be acute or more slow and insidious to develop.
Clinical Signs: reluctant to walk, walking very stiffly or as if walking on “eggshells”, lying down more often than normal, constantly shifting weight from one foot to another, and/or rocking back or “sitting” on his or her hindquarters. A full physical exam and bloodwork is required for to determine possible causes and treatment.
What to do: Confine the horse in a deeply bedded stall, ice the horse’s feet, stop feeding grain or treats of any kind and DO NOT allow access to grass.
Laminitis is a potentially life-threatening situation that should be taken seriously. Prompt veterinary attention is essential to a positive outcome.
A.D.R’S:
Ain’t doin’ right emergencies. This ADR category is a rather vague and nebulous one. It is one where clients most commonly say “He/she just isn’t right. I know something is wrong.”
Clinical Signs: low grade fever, anorexia, lethargy, and or mild colic.
What to do: Call your veterinarian and discuss the symptoms of your ADR. Sometimes it requires a physical exam and blood work to diagnose your horse’s condition. It may be mild colic or as severe as liver or kidney disease.

Neurologic Signs:
Common causes of neurologic signs are EEE/WEE, West Nile Virus, Neurologic herpesvirus (EHV-1), Equine Protozoal Myelitis (EPM), trauma to the head or spinal cord or Wobbler’s syndrome in young horses. Neurologic cases can only be diagnosed with special tests.
Clinical Signs: Stumbling, Loss of balance, incoordination, unable to chew or swallow, droopy lid or ear, severe depression, unresponsive to stimulation, compulsive circling, head pressing, acute onset of blindness. These symptoms may or may not have a fever associated with them.
What to do: Minimize contact with the affected horse. Always wear gloves and quarantine neurologic horses from other horses until a definitive diagnosis is reached. Unbalanced/uncoordinated horses are extremely dangerous and extreme care must be used when handling them. When your veterinarian arrives a thorough neurologic exam will be performed and appropriate blood test will be run.
In Summary
Preparation will help you stay calm in the event of an emergency. Keep your veterinarian’s phone number and your first aid kit handy. REMEMBER, in an emergency, time is critical. By acting quickly and promptly, you can minimize the consequences of an injury or illness. Your horse’s health and well-being depend on it.
Poisonous Pasture Weeds
Common Milkweed:
“Milkweed” is adequately named for the milky white juice that exudes from broken or cut stems or leaves. Milkweed is found throughout the United States in open, sunny areas. Milkweed produces galitoxin which is found in the vegetative parts of the plant. This is a cardiac glycoside that is toxic to horses. Symptoms include depression, irregular heartbeat, diarrhea, weakness, labored breathing, and even death. If you find milkweed in your pastures, the most effective method for removal from is hand pulling and removing the taproot. Mowing is not an effective management of milkweed.

Nightshades including Horse Nettle:
Toxic plants in the night shade family include: horse nettle (pictured), black nightshade, bitter-sweet nightshade, ground cherry, tomatoes and potatoes. Various species of nightshade are found in various parts of the US. Horse nettle is most commonly found in the NJ region. The leaves, shoots and unripe green berries all contain a glycoalkaloid called solanine. The unripe berries are the most toxic. Solanine affects the central nervous system and gastrointestinal tract. Symptoms include pupil dilation, diarrhea, inappetence, and loss of muscular coordination.

Horses would have to consume 1-10 pounds of horse nettle before showing symptoms of toxicity. Please note, in the fall the berries can turn to a red or yellow-orange color and is sometimes baled in hay. If you see the berries in your hay, remove them along with the dried plant material. Horses will not eat horse nettle unless they are very hungry and do not have access to quality alternative forage. Horse nettle is controlled with the timely application of herbicide during the flowering stage and prior to berry formation.

Pokeweed:
Pokeweed is native to the eastern United States. It is commonly found in pastures and along fence lines. It is 2 to 8 feet tall with white flowers that give way to purple-black berries. The stem is red or purple in color. The leaves exude an unpleasant scent when crushed. All parts of this plant especially the roots contain saponins and oxalates. Symptoms of toxicity include chronic colic and diarrhea. Pokeweed is not palatable to horses and will be avoided if provided access to good pasture and hay. Hand pulling is effective only if plants are small. Once a root system is established herbicides must be used to eradicate the plant.

Jimsonweed:
Jimsonweed is an annual herb that grows up to 5 feet tall and has a distinct “tree like” shape. The leaves are coarse and serrated. The seeds are contained in a hard spiny capsule. It grows in cultivated fields as well as overgrazed pastures. Jimsonweed is extremely toxic to both horses and humans. All parts of the plant are poisonous. Jimsonweed toxicity is caused by tropane alkaloids. Symptoms of jimsonweed poisoning include weak, rapid pulse, dilated pupils, rapid breathing, muscular twitching, inappetence, depression, incoordination, diarrhea, convulsions, coma, and possible death. Jimsonweed can accidentally be harvested with hay. Please note, that due to its strong odor and unpleasant taste, horses will usually avoid consuming jimsonweed as long as good quality forage is available. Management and control of jimsonweed is through herbicide treatment.

Buttercup:
Buttercup is found in meadows, pastures, and abandoned fields. Buttercups are easily identified by their slender hairy stem and yellow flower. The toxin is found in the leaves and flowers of the plant. Symptoms of toxicity include blistering of the mouth and skin. Swelling of the nose, lips and face may be ob-served after contact with the plant. Diarrhea and colic may occur if the plant is ingested. Buttercup is toxic when eaten fresh in pasture and loses toxicity when dried. Please note, if dried buttercup is found in the hay supply it is not normally toxic. Horse owners should be most concerned with consumption in the pasture. Since buttercup is most commonly found in overgrazed pastures, proper pasture management will help control or eliminate the infestation. Herbicide treatment is effective in treating buttercup infestations.

Hemp Dogbane:
This species is frequently found in pastures and can reach 5 feet in height. It reproduces through seed dispersal as well as clonal growth. Clonal growth occurs when horizontal roots creep underneath the soil service and send new plant growth up to the surface. Hemp dogbane contains small white flowers and both the leaves and stems contain a milky white sap. Hemp dogbane is easily confused with milkweed because they are so similar. The toxic sub-stance found in the leaves of the plants is a glycoside. Symptoms of toxicity include digestive upset, diarrhea, elevated temperature and pulse, sweating, dilated pupils, inappetence, and overall weakness. Dried dogbane that is accidentally baled in hay is also toxic. Controlling hemp dogbane in pastures is very difficult. Mowing is generally ineffective and herbicidal treatment might require multiple applications. Consult your local Cooperative Extension Service for assistance with herbicidal control.

In Summary:
In most cases horses will not consume these poisonous plant species as long as good quality forage is available. Keep pastures healthy by implementing a rotational grazing system and mowing weeds before they set seed. If pastures are sparse and rotational grazing is not an option consider providing a good source of hay as supplemental forage. Before applying any herbicides it may be useful to contact your local Cooperative Extension Agent. They will be able to perform a site visit and confirm the ID of the plant species and provide the appropriate herbicide to be applied to control it.
East Coast Equine Veterinary Service LLC
East Coast Equine is a fully ambulatory practice which services primarily Sussex, Warren, and Morris counties in Northern NJ. We provide all aspects of equine medicine, surgery, and dentistry with a special emphasis on sports medicine and lameness. Our services include preventative health care and general medicine, lameness diagnostics, pre-purchase examinations, dentistry, minor surgical procedures, emergencies, and reproductive services.
As technology in the field of veterinary medicine continues to advance, East Coast Equine will remain dedicated to maintaining a state of the art equine veterinary practice. The practice is equipped with cutting edge technology allowing the veterinarian to provide horse owners with the most progressive care available. The ambulatory units have access to digital ultrasonography and radiography as well as in field lap-tops allowing the veterinarian to have 24-7 access to any patient’s file.
